The global healthcare landscape has undergone a seismic shift in recent years, with remote healthcare technologies emerging as critical tools for delivering medical services. As health systems worldwide grapple with workforce shortages and increasing demand, identifying appropriate technologies for telemedicine has become more than just an operational consideration – it's a matter of public health imperative.
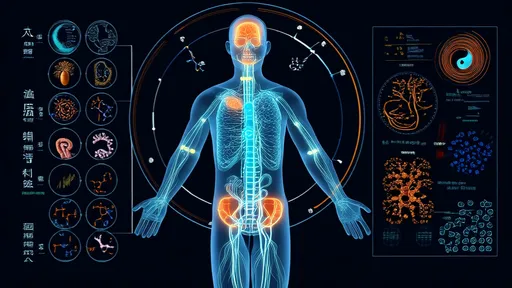
Defining the technological backbone of modern telemedicine requires understanding both clinical needs and practical limitations. The ideal remote health technologies must bridge physical gaps without compromising care quality, while remaining accessible across diverse socioeconomic contexts. From simple SMS-based appointment reminders to sophisticated AI-powered diagnostic tools, the spectrum of appropriate technologies varies dramatically based on local infrastructure and healthcare priorities.
Core infrastructure forms the foundation of any telemedicine program. Reliable internet connectivity, while obvious, remains unevenly distributed globally. Interestingly, some of the most impactful telemedicine implementations in low-resource settings have leveraged basic mobile networks rather than high-bandwidth solutions. This pragmatic approach highlights how appropriateness depends more on reliability and coverage than technical sophistication.
Patient-facing technologies represent the most visible component of remote healthcare. Secure messaging platforms have proven particularly versatile, serving functions from prescription renewals to mental health support. Video consultation tools, while resource-intensive, provide the closest approximation to in-person visits. However, asynchronous "store-and-forward" systems often demonstrate better suitability for specialist consultations in areas with unreliable connectivity.
The diagnostic capabilities of remote medicine have expanded dramatically. Portable digital stethoscopes, smartphone-connected otoscopes, and AI-assisted imaging analysis tools now enable comprehensive physical examinations at a distance. These technologies gain particular relevance in chronic disease management, where regular monitoring can prevent costly hospitalizations. Surprisingly, some of the most impactful diagnostic tools remain decidedly low-tech, such as standardized photography protocols for wound assessment.
Data integration challenges persist as a critical consideration. Appropriate telemedicine technologies must interface with existing electronic health records while maintaining rigorous security standards. The most successful implementations often use modular systems that can adapt to various health IT environments rather than demanding complete system overhauls. Interoperability emerges as a key determinant of long-term viability for any telemedicine technology.
Special populations require tailored technological solutions. Pediatric telemedicine benefits from engagement tools like digital toys that facilitate remote developmental assessments. Geriatric applications increasingly incorporate fall detection sensors and medication adherence monitors. For rural populations, hybrid models combining community health workers with specialist tele-support often outperform purely technological solutions.
Regulatory compliance shapes the appropriateness landscape significantly. Technologies must satisfy regional data protection laws, medical device regulations, and professional practice standards. This regulatory complexity explains why some apparently superior technologies see limited adoption – the compliance burden outweighs potential benefits. Successful programs typically adopt technologies with built-in compliance features rather than attempting to retrofit solutions.
The economic dimension cannot be overlooked when assessing technological appropriateness. Total cost of ownership extends far beyond initial purchase prices to include training, maintenance, and opportunity costs. Some healthcare systems have achieved remarkable outcomes using repurposed consumer technologies, while others found specialized medical devices more cost-effective in the long run. Sustainability depends on aligning technological choices with reimbursement models and organizational priorities.
Workflow integration often determines success more than technological features. Appropriate solutions must complement rather than disrupt clinical routines. The most adopted technologies typically minimize additional steps for providers while maximizing clinical value. This explains the popularity of integrated platforms over best-of-breed solutions in many implementations, despite theoretical advantages of specialized tools.
Emerging technologies continue to reshape the appropriateness calculus. AI triage systems, blockchain-based health records, and augmented reality visualization tools show promise but face adoption barriers. The pandemic accelerated acceptance of many innovations, but lasting adoption requires evidence of improved outcomes rather than just technical feasibility. Interestingly, some older technologies like interactive voice response systems have seen renewed relevance due to their accessibility.
The human element remains paramount in technology selection. Systems that enhance rather than replace clinician-patient relationships tend to achieve better outcomes. Appropriate technologies facilitate empathy and trust across digital mediums – a consideration that often gets overshadowed by technical specifications. Successful implementations typically involve end-users in technology selection processes.
Looking ahead, the telemedicine technology landscape will continue evolving rapidly. The most appropriate solutions will balance innovation with reliability, sophistication with accessibility, and capability with usability. As healthcare delivery becomes increasingly decentralized, the technologies that endure will be those that serve both clinical and human needs equally well. The future of remote healthcare belongs to technologies that disappear into the background, letting healing relationships take center stage.

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025