The concept of immunonutrition has gained significant traction in postoperative care, particularly for patients recovering from major surgeries. The interplay between nutrition and immune function is complex, yet undeniably critical for optimal recovery. Surgical stress triggers a cascade of metabolic and immunological changes that can deplete the body's resources, leaving patients vulnerable to infections, delayed wound healing, and prolonged hospital stays. Immunonutrition aims to counteract these effects by providing targeted nutrients that modulate immune responses, enhance tissue repair, and reduce inflammation.
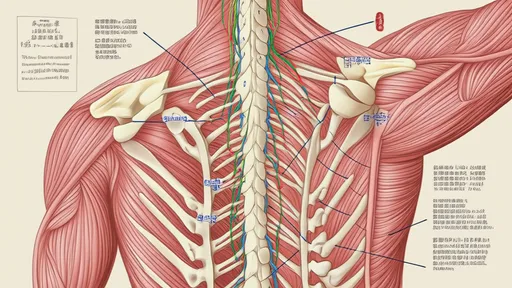
Understanding the physiological impact of surgery is essential to appreciate why immunonutrition matters. The trauma of an operation activates the body's stress response, leading to increased energy expenditure, protein breakdown, and a surge in inflammatory cytokines. This hypermetabolic state can persist for days or even weeks, depending on the severity of the procedure. Malnutrition, whether pre-existing or acquired during hospitalization, exacerbates these challenges. Patients with inadequate nutritional status are more likely to experience complications such as surgical site infections, sepsis, and organ dysfunction. Immunonutrition seeks to address these risks by supplying key substrates that support immune cell function and promote anabolic processes.
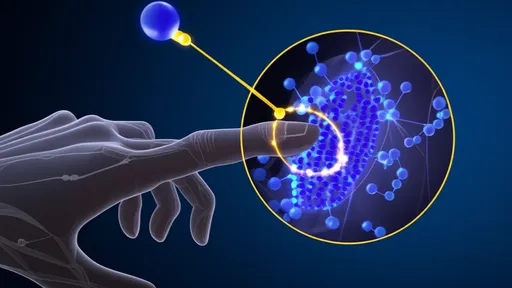
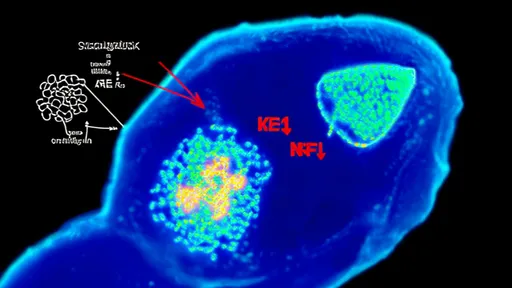
The cornerstone of immunonutrition lies in its bioactive components. Certain amino acids, fatty acids, vitamins, and minerals have been shown to exert immunomodulatory effects. For instance, arginine plays a dual role as a precursor for nitric oxide synthesis and a stimulant for T-cell proliferation. Glutamine, another conditionally essential amino acid during stress, serves as fuel for enterocytes and immune cells. Omega-3 fatty acids, derived from fish oil, possess potent anti-inflammatory properties that can mitigate excessive postoperative inflammation. Antioxidants like vitamins C and E help neutralize free radicals generated during oxidative stress. These nutrients work synergistically to create a favorable environment for healing.
Clinical evidence supporting immunonutrition continues to accumulate across various surgical specialties. Studies in gastrointestinal, cardiac, and cancer surgeries have demonstrated reductions in infection rates, shorter lengths of stay, and improved wound healing when immunonutrition protocols are implemented. The timing of intervention appears crucial—initiating supplementation preoperatively may prime the immune system, while postoperative administration sustains the benefits. Enteral delivery is generally preferred over parenteral routes when feasible, as it preserves gut barrier function and reduces the risk of bacterial translocation. However, individualized approaches are necessary, considering factors like the patient's baseline nutritional status, type of surgery, and potential contraindications to specific nutrients.
Practical implementation of immunonutrition requires multidisciplinary collaboration. Surgeons, dietitians, and pharmacists must work together to identify candidates who would benefit most from these interventions. Standardized protocols help ensure consistency, but flexibility is needed to accommodate patient-specific variables. Monitoring parameters such as inflammatory markers, nitrogen balance, and clinical outcomes allows for timely adjustments. While immunonutrition formulas are commercially available, their cost-effectiveness must be weighed against potential savings from reduced complications. Patient education also plays a vital role, as adherence to oral supplements can significantly influence results.
Despite its promise, immunonutrition is not without controversies and limitations. Questions remain about optimal nutrient combinations, dosages, and duration of therapy. Some studies have failed to replicate the dramatic benefits seen in earlier trials, suggesting that patient selection and methodological differences may affect outcomes. Concerns have been raised about excessive arginine supplementation in septic patients, potentially worsening hemodynamic instability. Additionally, access to specialized formulas may be limited in resource-constrained settings. Ongoing research aims to refine protocols and identify biomarkers that predict responsiveness to immunonutrition.
The future of postoperative immunonutrition may lie in personalized approaches. Advances in nutrigenomics could enable tailored interventions based on genetic predispositions to inflammation and metabolic responses. Probiotics and prebiotics might be incorporated to optimize gut microbiota, which plays an emerging role in immune regulation. The integration of immunonutrition with enhanced recovery after surgery (ERAS) pathways represents another promising direction. As our understanding of the gut-immune axis deepens, novel therapeutic targets may emerge, further bridging the gap between nutrition science and clinical practice.
In conclusion, immunonutrition represents a paradigm shift in postoperative care, moving beyond traditional nutritional support to actively influence immune competence. While not a panacea, it offers a scientifically grounded strategy to improve surgical outcomes, particularly in high-risk patients. The art lies in judicious application—recognizing when and how to employ these specialized nutritional interventions to maximize benefit. As research progresses, immunonutrition will likely become more sophisticated, cementing its role as an integral component of perioperative medicine.

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025