For centuries, acupuncture has been shrouded in both reverence and skepticism. While traditional Chinese medicine explains its effects through concepts like qi and meridians, modern science has struggled to validate these ancient claims. However, recent advances in neuroimaging technologies are finally providing concrete evidence about what actually happens in the brain during acupuncture treatment.
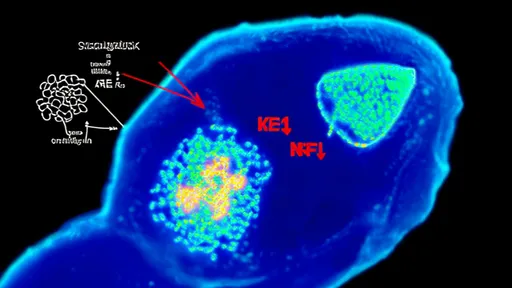
Functional magnetic resonance imaging (fMRI) studies have revealed that acupuncture stimulation triggers measurable changes in brain activity patterns. Unlike the vague "energy flow" descriptions of traditional texts, these scans show precise neurobiological responses. The needle insertion appears to modulate activity in specific brain regions associated with pain processing, emotional regulation, and autonomic control.
The most compelling findings come from pain research. When acupuncture needles are applied to recognized points, fMRI scans consistently show decreased activity in the anterior cingulate cortex and insula - brain areas known to process pain perception. Simultaneously, increased activation occurs in the prefrontal cortex and periaqueductal gray, regions involved in pain inhibition. This provides a neurological explanation for acupuncture's analgesic effects that aligns with Western understanding of pain pathways.
Beyond pain management, neuroimaging studies demonstrate acupuncture's influence on the limbic system. The amygdala, hippocampus, and hypothalamus all show altered activity patterns during treatment. These structures govern emotional processing and stress responses, potentially explaining why many patients report improved mood and reduced anxiety after acupuncture sessions. The timing of these brain changes correlates closely with reported subjective improvements, strengthening the case for a genuine biological effect.
Interestingly, research comparing real and sham acupuncture reveals distinct neural signatures. While both may show some brain activity changes due to placebo effects, genuine acupuncture produces more extensive and sustained modulation of functional connectivity between brain regions. This helps distinguish specific therapeutic effects from nonspecific factors. The differences are particularly pronounced when using traditional acupuncture points versus random needle placement.
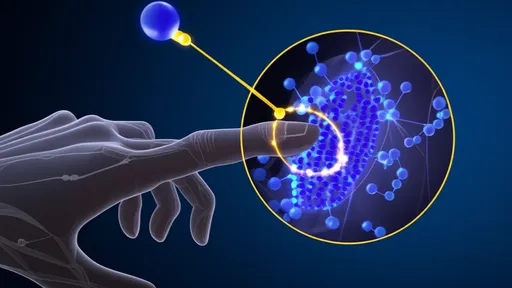
Neurochemical changes accompany these brain activity patterns. Positron emission tomography (PET) scans have detected acupuncture-induced alterations in opioid receptor availability and dopamine release. This provides molecular-level confirmation of what practitioners have observed clinically for generations - that acupuncture can produce natural pain-relieving and mood-enhancing effects similar to pharmaceutical interventions but without the side effects.
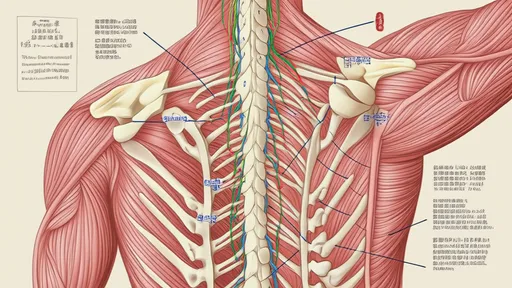
The autonomic nervous system also appears to be a key mediator of acupuncture's effects. fMRI studies demonstrate that certain acupuncture points can selectively modulate parasympathetic or sympathetic activity, as reflected in changes to the hypothalamus and brainstem nuclei. This may explain acupuncture's ability to regulate diverse bodily functions from digestion to blood pressure through central nervous system control.
Perhaps most intriguing are findings about acupuncture's cumulative effects. Single sessions show immediate but transient brain changes, while repeated treatments lead to lasting neuroplastic adaptations. Longitudinal studies reveal structural changes in gray matter density and white matter integrity in regions corresponding to patients' symptom improvements. This suggests acupuncture doesn't just temporarily mask symptoms but may facilitate genuine neural reorganization.
Critics argue that some observed effects could result from expectation rather than specific needle actions. However, studies controlling for placebo factors, including those using animal models, continue to find distinct neurological changes. Moreover, the spatial specificity of responses - with different points activating different brain networks - supports traditional acupuncture point localization in a way that challenges purely psychological explanations.
Current research is exploring how these neuroimaging findings can optimize treatment. By identifying which brain patterns predict good clinical responses, practitioners may eventually personalize point selection based on individual neural signatures. Some researchers are even investigating whether combining real-time fMRI feedback with acupuncture could enhance therapeutic outcomes through neurofeedback mechanisms.
As the body of neuroimaging evidence grows, it's creating an unprecedented bridge between Eastern healing arts and Western medicine. The scans don't necessarily validate traditional Chinese medicine theories in their original form, but they do confirm that acupuncture produces measurable, specific effects on brain function. This convergence of ancient practice and modern technology may finally provide the common language needed to integrate acupuncture more fully into mainstream healthcare.
The implications extend beyond acupuncture itself. Understanding how mechanical stimulation at peripheral points can influence central nervous system function could revolutionize our approach to neuromodulation therapies. As research continues, we may discover even more about the brain's remarkable capacity to heal itself when properly stimulated - whether through needles, pressure, or other forms of somatic intervention.

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025